News and Award
About CMUH
Acute Pulmonary Embolism (APE) could be fatal. Thrombosis by Ultrasonic Homogenization Combined with Catheter-Directed Thrombolysis Therapy. Up to 95% thrombolysis success rate and reduces intracerebral hemorrhage
Have you ever suffered from shortness of breath or chest tightness but could not find the reason or stopped paying attention after the symptoms have been alleviated? Be careful, this could be caused by “acute pulmonary embolism (APE).” Acute pulmonary embolism (APE) is a type of rare etiology easily neglected from diagnosis, which causes shortness of breath or chest tightness. Hence, acute pulmonary embolism is also known as the “great makeup artist.” There is a danger in massive pulmonary embolism that could often affect the blood pressure, heartbeat and oxygen concentration of blood, endangering the life and even requiring Extra-Corporeal Membrane Oxygenation (ECMO) to survive from the acute phase.
Ultrasound Homogenization + Catheter-Directed Thrombolysis (CDT) successfully rescues endangered patients
CMUH Division of Cardiology, Section of Peripheral Vessels Director Chung-Ho Hsu suggests that such massive pulmonary embolism could lead to high risk of sudden cardiac death due to the influence on blood pressure and oxygen concentration in blood. The corresponding treatment must be done within the golden window for rescue and will require immediate thrombolysis after making a finite diagnosis; or else the mortality rate will fall between 50% and 80% if the thrombosis is only removed by surgery for emergency rescue. Thrombosis by ultrasound homogenization combined with catheter-directed thrombolysis has successfully saved many endangered patients.
Up to 95% in thrombolysis success rate
Chung-Ho Hsu proposes the following modes of therapies after the finite diagnosis of acute pulmonary embolism (APE), including: (1) General thrombolytic agent by intravenous injection: However the thrombosis removal rate is low and most importantly such therapy involves high risk of intracerebral hemorrhage. (2) Other modes mainly consist of catheter-directed thrombolysis. CMUH treats acute pulmonary embolism (APE) through extending a micro catheter via the veins from the groin into the pulmonary artery, placing the thrombolysis catheter and providing thrombolysis agent locally to substantially lower the risk of intracerebral hemorrhage. The treatment can also achieve the thrombolysis effect more effectively.
The following two examples are actual patient cases applied with such technology, namely inducing the ultrasound energy into the thrombolysis catheter to homogenize thrombosis while injecting the dose of thrombolytic agent locally, which resulted in over 95% thrombolysis effect. It is also an extremely-low risk therapy for intracerebral hemorrhage with excellent performance in thrombolysis effect, which is much higher than the 60-70% thrombolysis success rate in conventional therapy. Therefore the public is reminded not to overlook the severity of shortness of breath and chest tightness without identified reason. Be careful, as it could be pulmonary embolism and early diagnosis and therapy are necessary.
Here are two cases we would like to share with you:
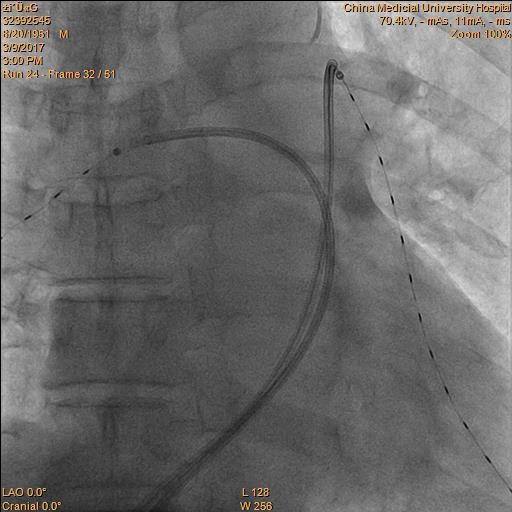
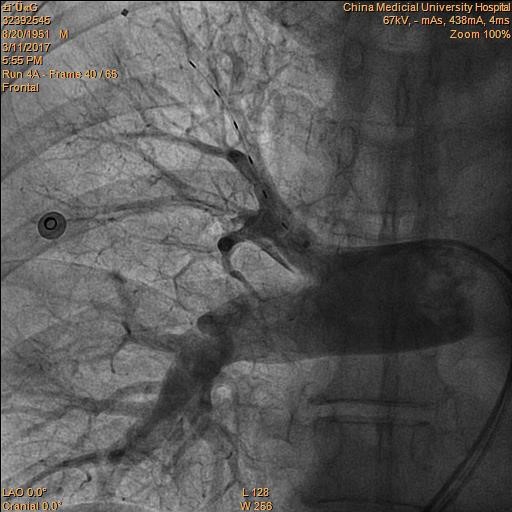
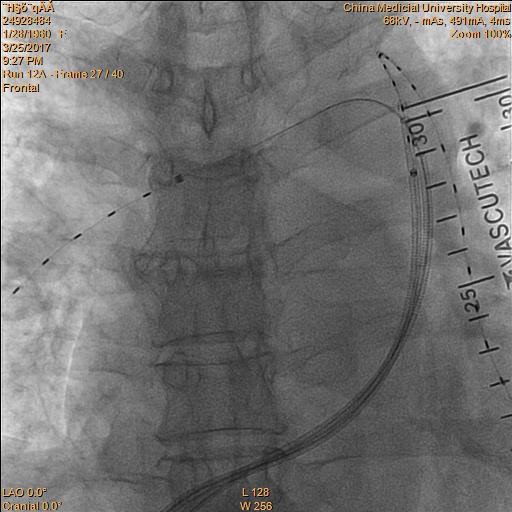
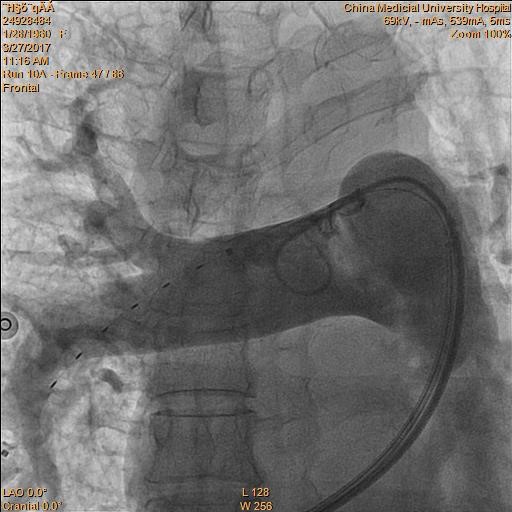
(Case 1) Patient Mr. Zhang, 65 years old, took laser-assisted transurethral resection for benign prostatic hypertrophy in our hospital earlier this January. After a few days of bed rest, the patient suffered from shortness of breath in activities for 1.5-2 months and later the condition deteriorated with aggravated wheezing. The patient went to CMUH for treatment, whose blood pressure showed 162/100 mm Hg at the emergency room, heart rate at 121 beats per minute and shortness of breath. The patient was treated with Bi-level Positive Airway Pressure (BIPAP) at the ICU and was discovered with massive acute pulmonary embolism (APE) on the two side through CT examination (Figure 1). The patient was placed with EKOS thrombolysis catheters on the two sides under emergency thrombolysis at ICU (Figure 2), the pulmonary artery imaging shows effective thrombolysis of blood clots (Figure 3). The wheezing symptoms of the patient improved and the patient was discharged from the hospital in about one week.
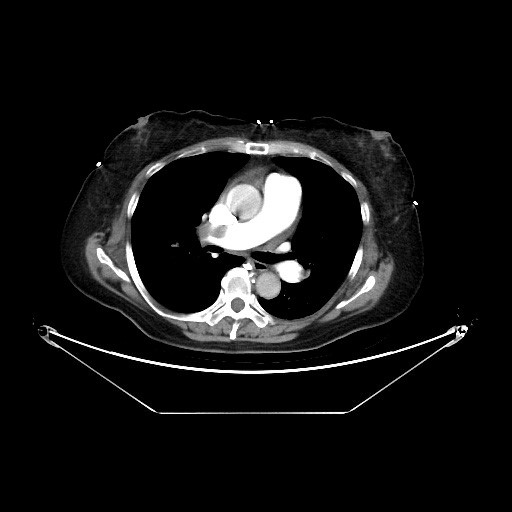
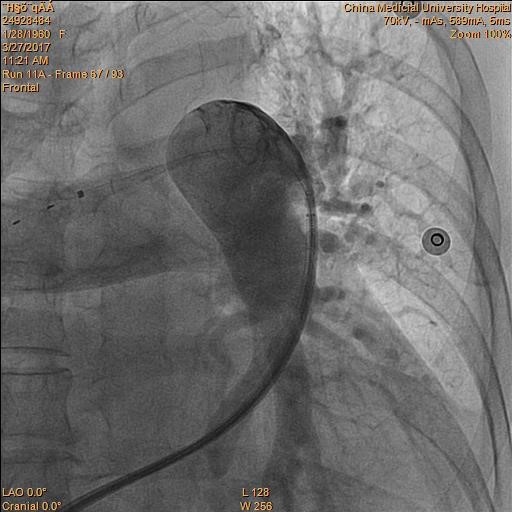
(Case 2) Patient Ms. Shen, 57 years old, experienced wheezing in activities in the previous two to three months prior to hospitalization. The patient could not be found of finite cause of disease during outpatient follow-up and the condition deteriorated with aggravated wheezing. The patient was then treated at emergency room of CMUH, whose oxygen concentration in blood drooped to 92% at the ER. After taking the CT examination, the patient was discovered massive acute pulmonary embolism (APE) on the two sides (Figure 4). The patient was placed with EKOS thrombolysis catheters on the two sides under emergency thrombolysis (Figure 5), the pulmonary artery imaging shows effective thrombolysis of blood clots (Figure 6). The wheezing symptoms of the patient improved and the patient was discharged from the hospital in about one week.
(Figure 1) (Figure 2)
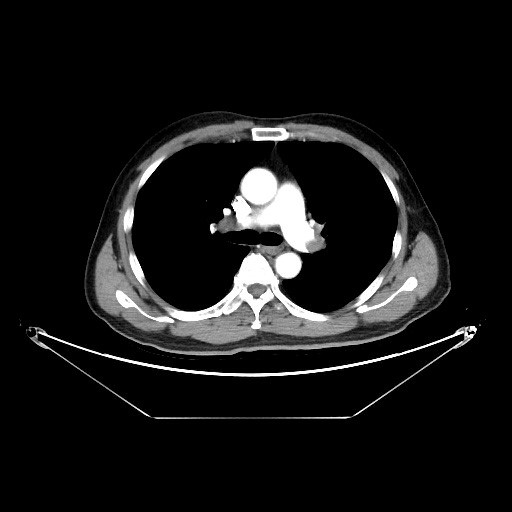
(Figure 3)
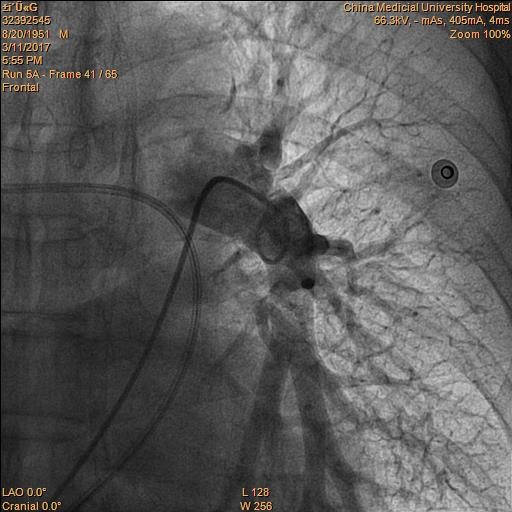
(Figure 4) (Figure 5)
(Figure 6)
Section of Peripheral Vessels, Division of Cardiology / Director Chung-Ho Hsu



![[Taiwan–Malaysia Medical Innovation Forum] CMUH and UNIMAS Co-Host Major Medical Symposium to Advance Medical Technology and Precision Patient Care img](/FileUploads/News/20250714_131324.jpg?w=250&h=180&mode=crop&scale=both)